Its called a Haglund’s deformity or a pump bump. Ice skaters call it a Bauer bump (after the most popular brand of ice skates).
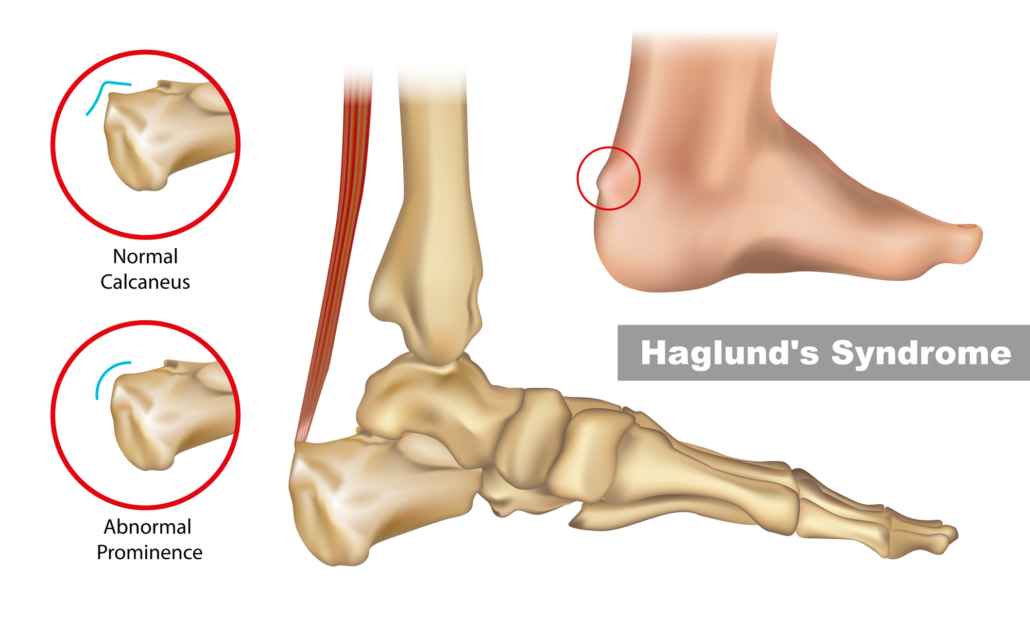
Everyone has some amount of enlargement at the back of the heel bone. Some just have more or less than others. It is a natural and natural variation. However, those who have a larger bump are going to have problems with pressure from the shoes, especially if the nature of the footwear used is rigid (eg ice skates). This then becomes painful and a swollen bursitis may develop, resulting in the problem of Haglund’s deformity.
The best way to treat a Hauglund’s deformity is to get out of the shoes that are causing the problem. If that is not possible, then try to get into footwear that is not rigid and somewhat flimsy in the heel counter.
Felt padding can be used to make pads the shape of a horseshoe or a donut with a hole in it to get the pressure from the shoe off the painful area. There a also silicon gel Haglund’s protector pads that are a sleeve around the ankle that can be worn under the socks can be used to prevent friction.
If you have a problem with pain at the back of the heel and its not getting better, please give us a ring and we can help.